Maria was presented with this award in recognition of her collaboration with the Australasian College of Dermatologist and her contribution to dermatology nurse education as the author of the materials for the Certificate of Melanography Essentials. The online course has standardised melanography practice thereby providing a standard for future practice, that will be regularly revised and up-dated. This is a short article on one of her many areas of practice she is passionate about.
Maria Buckingham was presented with this award in recognition of her collaboration with the Australasian College of Dermatologist and her contribution to dermatology nurse education as the author of the materials for the Certificate of Melanography Essentials. The online course has standardised melanography practice thereby providing a standard for future practice, that will be regularly revised and up-dated. This is a short article on one of her many areas of practice she is passionate about.
DERMOSCOPY DECONSTRUCTED

Dermoscopy is the visualisation of the sub surface structure of pigmented naevi and other skin lesions. It has become routine practice with dermatologist and in primary care skin cancer practitioners for use in the earlier detection of melanoma and non-melanoma skin cancer. Widespread adoption of dermoscopy has been made possible due to the introduction of handheld dermatoscopes.
An increasing number of nurses use dermatoscopes in their day to day work when examining patients’ skin and the process of melanography (lesion triage and dermoscopic imaging) requires that the nurse is competent in dermoscopic lesion pattern assessment.
This article explains the two basic elements of dermoscopy and outlines lesion pattern analysis in reference to anatomy.
A dermatoscope is a device similar to an otoscope which uses magnification and strong, directed light to minimise skin surface glare thereby rendering transparency through the normally opaque surface layer of the skin.
Light
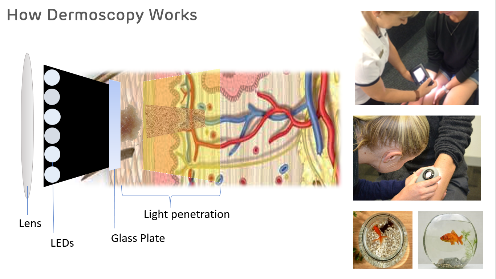
The light source used in dermatoscopes are light emitting diodes (LEDs). Most modern dermatoscopes have cross polarised light and some have dual features of cross polarised and non-polarised light.
The cross polarisation increases light rays concentration, minimising surface light scatter, and enabling clearer visualisation of patterns and colours and vasculature in the epidermis and dermis. Non polarisation provides more superficial examination of keratin structures. The depth of visualisation is between 3-5mm through the epidermis to the dermis.
Contact and non-contact dermatoscope
Dermatoscopes have contact or non-contact modes. Some dermatoscopes have both mode options.
Contact dermatoscopes are placed directly on the skin, providing greatest clarity due to minimal light scatter. Using a fluid interface (alcohol or oil) further enhances visibility.
Non-contact dermatoscopes are held about 10mm away from the skin and provide excellent visibility, they require no fluid interface but are minimally more difficult to master due to ability to judge the correct distance from the skin. It is of especial benefit for inspecting lesions in personal areas such as buttocks and genital areas as accurate inspection without direct contact to the skin or mucosal surface.
Dermoscopy explained

Dermoscopy could be said to be a party trick with light! A surprising feature of the epidermis and dermis layers of the skin is that they are relatively transparent, except for the epidermal stratum corneum, therefore when a light is placed behind the fingers in the dark, it is possible to see light shining through parts of the skin, despite obvious opaqueness in normal light. The dermatoscope utilises the same physiological phenomenon to penetrate the normally opaque skin surface.
Dermoscopic light penetrates the opacity of the stratum corneum to visualise the patterns and colours at different depths beneath. An analogy of dermoscopy is gazing into the top of a goldfish bowl where everything appears on one level but, viewing the bowl from the side it is evident that the fish, plants and gravel are located at different levels in the bowl.
Features and patterns visualised in dermoscopy
Dermoscopic pattern recognition is an important skill to master to perform confident lesion assessment.
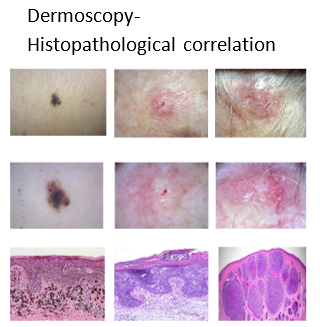
Colour of features: Colour generally signifies melanin pigment deposits in the different layers of the epidermis and dermis. Darker or larger pigmented structures indicate higher pigment concentration due to increased melanocytic activity whereas aggregated grey or blue dots and lines indicate melanin deposits in the papillary and reticular dermis which are not generally present. Other colours may be seen as non-pigmented (white, pink or red) or as vessel structures (varying from red to purple).
Correlation of dermoscopic features and histopathological structures and the significance of features for the identification of melanoma specifically and also in non-melanoma skin cancers has been empirically confirmed. Asymmetry of colour deposit or irregular patterns and structures indicate chaos which provides clues to malignancy.
Dermoscopy uses a combination of magnification and LED lights and a handheld dermatoscope is used in both specialist and primary care skin cancer practice. Increasingly dermoscopy is utilised by dermatology nurses. Empirical studies have confirmed correlation between dermoscopy and histopathological features. It is recognised as an essential tool for accurate and earlier identification of features of melanoma and non-melanoma skin cancer.
References
Oakley, A. (2004). Dermoscopy. Available: https://www.dermnetnz.org/topics/dermoscopy/. Last accessed 8th March 2020.
Yung, A. (2007). Dermatoscope Overview. Available: https://www.dermnetnz.org/topics/dermatoscope-overview/. Last accessed 6th March 2020.
Buckingham, M. (2017). Dermoscopy Deconstructed: Magnification, Light and the Skin. Course material, Certificate of Melanography Essentials, Australasian College of Dermatologists. https://acdcourses.dermcoll.edu.au/
Goldman, L., Yoijnker, W. (1946). Studies In Microscopy Of The Surface Of The Skin. Preliminary Report of Technics 1 2.
Ferrara G, Argenyi Z, Argenziano G, Cerio R, Cerroni L, Di Blasi A, Feudale EA, Giorgio CM, Massone C, Nappi O, Tomasini C, Urso C, Zalaudek I, Kittler H, Soyer HP (2009) The influence of clinical information in the histopathologic diagnosis of melanocytic skin neoplasms. PLoS One. 2009;4(4):e5375. doi: 10.1371/journal.pone.0005375. Epub 2009 Apr 30.
Russo, T., Piccolo, V., Ferrara, G., Agozzino, M., Alfano, R., Longo, C., Argenziano, G. (2017) Dermoscopy pathology correlation in melanoma. Journal of Dermatology, Journal of Dermatology 2017; 44: 507–514. RCH 01, 2002
Kittler, H., Pehamberger, H., Wolff, K., Binder, M. (2002) Diagnostic accuracy of dermoscopy
The Lancet Oncology, Volume 3:3, 159–65. 2002 DOI: https://doi.org/10.1016/S1470-2045(02)00679-4
Kittler H., Rosendahl C., Cameron A., Tschandl P. (2011) Dermatoscopy. An algorithmic method based on pattern analysis. 2011. Facultas Verlags and Buchhandels AG, Universitatsverlag, Austria.
Menzies S.W., Crotty, K.A., Ingvar, C. (2009) An Atlas of Surface Microscopy of Pigmented Skin Lesions: Dermatoscopy (3rd Edition) 2009; pp.13-14. McGraw-Hill Book Company, Australia.
Pehamberger H., Binder M., Steiner A., Wolff K. (1993) In vivo epiluminescence microscopy: improvement of early diagnosis of melanoma. J Invest Dermatol. 1993; 100: 356S-362S.
Feroze Kaliyadan (2016) The scope of the dermoscope, Indian Dermatol Online J. Sep-Oct; 7(5): 359–363. Available: http://www.idoj.in/temp/IndianDermatolOnlineJ75359-1990201_053142.pdf. Last accessed 6th July 2018.
Kittler H, Riedl E, Rosendahl C, Cameron A. Dermatoscopy of unpigmented lesions of the skin: a new classification of vessel morphology based on pattern analysis. Dermatopathology: Practical & Conceptual 2007;14:3.